Women are frequently told to “Exercise your pelvic floor” or “Do your Kegels” during various life stages and for different pelvic health conditions. Often, women are given a leaflet by their health provider about pelvic floor exercises and are expected to continue them without further instruction or advice. However, are pelvic floor exercises as simple as this, and should they be given in such a ‘one size fits all’ approach?
The aim of this blog is to provide clarification about how you can exercise your pelvic floor to suit your individual needs in order to reduce pelvic health symptoms and restore function that has relevance to you.
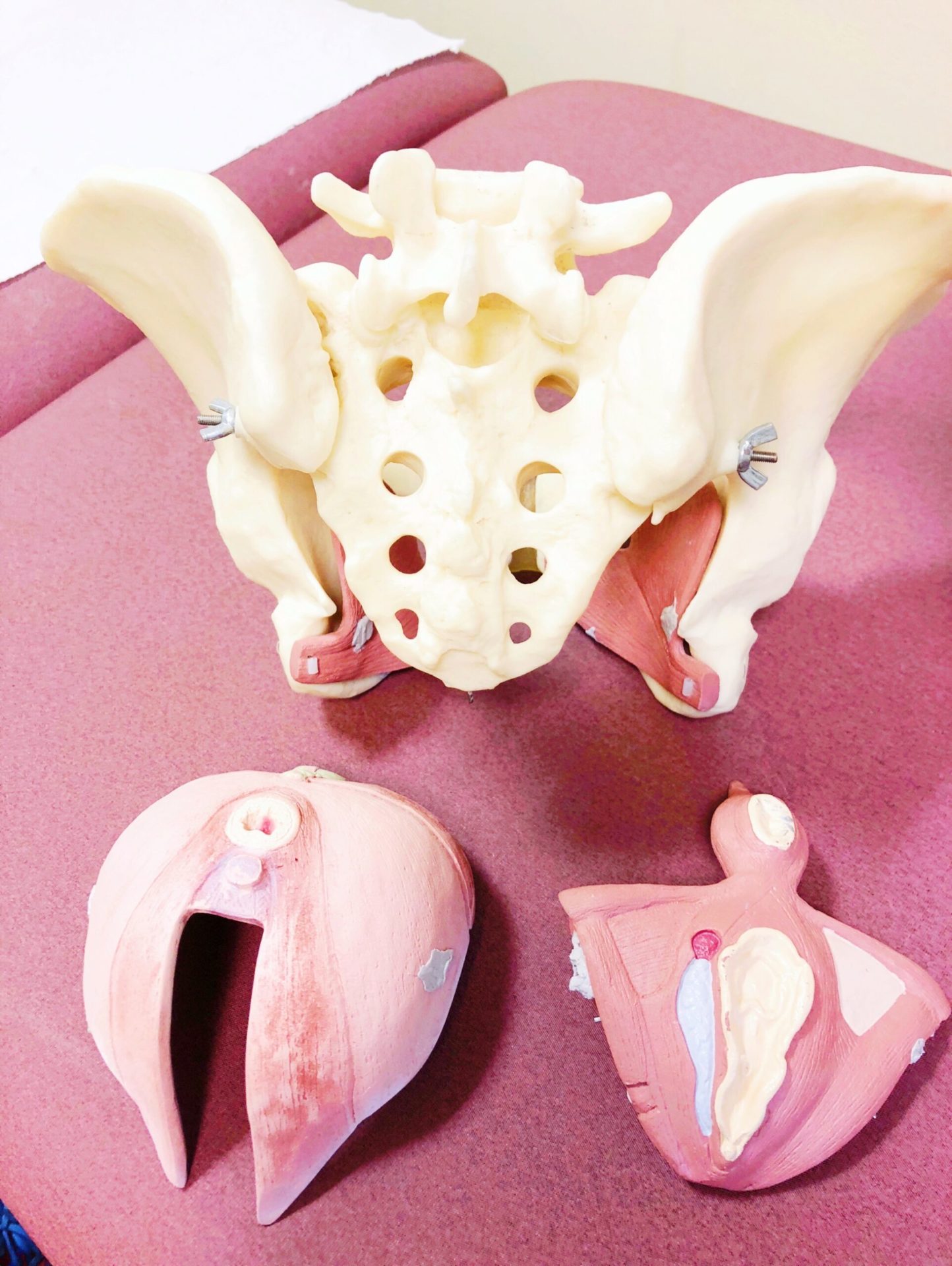
What and where are the Pelvic Floor muscles?
The pelvic floor muscles are situated at the base of the pelvis and form three layers of important muscle tissue, which play an essential role in supporting the organs within the pelvic cavity, maintaining continence, normal urination and defecation and sexual functioning.

Our previous blog post “Where is the pelvic floor, what does it do and why is it important?” details more about where these muscles are located and their specific functions – check out this blog post to find out further information enlivenhealth.co.uk/the-pelvic-floor-where-is-it-what-does-it-do-and-why-is-it-important
The deepest layer of pelvic floor muscle [the Levator Ani], help to support the pelvic organs and when they contract, they generate an upward and forwards ‘lift’ effect which help with this important role. This lift effect also results in a compressive, supporting force against the bladder, urethra and rectum to help maintain continence.
The superficial pelvic floor muscles work with the deepest layer of muscle as a functional unit, however these muscles also form an important part of continence maintenance by producing a ‘squeeze’ response when they contract, to assist with this function. Some of the muscles of these superficial layers also act as sphincters to help squeeze and close off the anus and urethra to prevent leakage.
Therefore, both the ‘squeeze’ and ‘lift’ muscular actions must be considered when pelvic floor exercise regimes are prescribed, in order to target both muscular layers.
The pelvic floor muscles are comprised of different types of muscle fibres which are made up of the contractile units of the muscles. 70% of these muscle fibres in the pelvic floor are called Type 1 fibres, which are slow twitch fibres, meaning that they can maintain a low level of contraction for long periods of time. This is important within the pelvic floor as the muscles must always uphold a level of tone in order to support the structures in and around the pelvic cavity, and to constantly maintain continence throughout the day. The remaining muscle fibres are termed Type 2 fibres, and these are capable of short, sharp, stronger contractions, important for sudden or more strenuous movements and for maintaining continence in instances of sudden increases of intra-abdominal pressure such as coughing, laughing or sneezing or during impact exercise.
The Pelvic Floor muscles must be able to contract both voluntarily and automatically without you having to think about it, in order to function normally.

What can cause Pelvic Floor Dysfunction?
Several factors can lead to problems within the pelvic floor musculature. These can affect how the muscles are able to work and can result in some of the following problems or symptoms:
- Urinary Incontinence
- Urinary urgency and/or frequency
- Fecal incontinence/urgency
- Constipation
- Pelvic Organ Prolapse
- Pain or problems with sexual intercourse
- Problems with passing urine or stool
Some of the common causes of Pelvic floor dysfunction include:
Pregnancy and Birth
The hormonal and postural changes which occur during pregnancy can have a weakening effect upon the pelvic floor. The weight of a growing baby, along with lengthening of muscle and stretching of the core muscles, places considerable strain on the pelvic floor and its associated soft tissues.
During delivery, over-stretching of the pelvic floor muscles and fascia [soft tissues] occur, which may cause damage to these structures and their associated nerves. A long pushing stage during labour, and delivery via forceps are considered risk factors for increased pelvic floor trauma and so are more likely to result in muscular dysfunction.

Lifestyle Factors
Like any muscle within the body, the pelvic floor is affected by lifestyle and use versus disuse or misuse.
Obesity has been shown to have a significant impact on pelvic floor function and is linked with Urinary Incontinence and Pelvic Organ Prolapse. This is because increased weight is linked with increased pressure within the abdomen and this causes strain and stress upon the muscles and the fascia within the pelvis, causing these structures to stretch and weaken. Weight loss programs have been shown to be effective in the management of incontinence in overweight women.
Aging processes
Aging in women is associated with a reduction in the hormone oestrogen. This hormone is important in pelvic health and its decline may result in the onset of symptoms, particularly during the peri and post-menopausal years. Reduced oestrogen levels may result in changes in collagen structure and muscle fibre numbers within the muscles, reducing muscle mass and strength.
Other
Other factors which have been suggested to influence pelvic floor health include ethnicity, the number of deliveries a woman has had, a history of pelvic surgery, chronic coughs, spinal cord disorders, family history, and genetics and chronic constipation.
What are we trying to achieve with Pelvic Floor exercises?
The primary aim of Pelvic Floor muscle training is to improve the muscle’s ability to work and function normally, whilst improving or curing the symptoms of pelvic health disorders such as urinary incontinence or prolapse. For the pelvic floor to work optimally it must:
- Be strong
- Have good endurance
- Be able to provide support to the pelvic structures
- Be able to contract and relax through its entire range
- Be able to be well-timed and well-co-ordinated during daily activities
- Be able to work normally in an automatic way, without you having to think about it
The effects of muscular strengthening exercise have been widely researched but are not yet fully understood. We know that when you exercise a muscle it is capable of change or ‘plasticity’, through both changes in nerve function to and from the muscle and through structural changes within the muscle itself. Exercise can increase the size of muscle fibres and it can change fibres from one type into another, depending on the type of exercise performed and the type of load which is applied to it. Muscle tissue may increase in size after 8 to 12 weeks of strengthening exercise and is capable of becoming thicker [or ‘hypertrophy’], remodelling and stiffening, even when it has been significantly damaged.
Neurological changes brought about through exercise include improved co-ordination, improved automatic reflex activation and learning, through the practice of specific exercise, which suits the individual and their goals.
Thus, the aims of a pelvic floor exercise program should be tailored to suit the goals of the individual and the specific problems they are presenting with, in order to bring about appropriate changes which will benefit them.
But do Pelvic Floor Exercises even work?
Research studies have shown that daily exercise of the pelvic floor for 6 months can result in increasing muscle thickness and stiffness, as well as providing improved support to the bladder and rectum.
The National Institute of Health and Care Excellence advises that Pelvic Floor Muscle Training should be the first line of treatment for Stress or Mixed Urinary Incontinence and for Pelvic Organ Prolapse. This is because there have numerous research trials carried out over the years which have found that Pelvic Floor Muscle Training can improve or cure the symptoms of these conditions in many women. Pelvic Floor muscle Training is also very important during pregnancy and in the postnatal period, to prevent and manage urinary incontinence and to assist in recovery after childbirth.
However, pelvic floor training protocols vary considerably across the research and so prescribing these exercises cannot be standardized to suit every woman, and so must be individualised according to her needs.

So, how should you be exercising your Pelvic floor?
We know from the research that in order for Pelvic Floor muscle training to work, women must be aware of the following:
- Supervised Pelvic Floor Muscle Training is more effective than unsupervised
- Exercises should be undertaken regularly [3 times a day for 3-6 months is the current recommendation]
- You have to do them for them to work!
- Exercise regimes must be progressed.
Exercise programs must be tailored to suit each individual, however they most commonly address muscle strength, endurance, timing and incorporation into functional activity.
A Women’s Health Physiotherapist will normally undertake an in-depth assessment of your pelvic floor function, by way of an internal examination. This will involve determining how strong your pelvic floor muscles are, if they are capable of a ‘lift’ as well as a ‘squeeze’, how long you can hold a contraction for, how many contractions you are able to do, and if the muscles contract automatically prior to a cough. They will also assess the muscle’s ability to relax, what their resting tone feels like and if there are any painful areas.
Once a full examination of the muscles and their function has been completed, a prescribed, individualised program to suit your ability and needs will be given to you, and this forms one of the key differences between seeing a Women’s Health Physiotherapist and being given a leaflet of exercises to do yourself at home.
However during the current state of ‘lockdown’ with the COVID19 outbreak and possible lack of accessibility to regular health services, it may be that a face to face session with a Women’s Health Physio is difficult at this time. The aim of the following information is to help guide you to locate and activate your pelvic floor yourself, so you may begin to exercise it without direct supervision. Should you experience any issues it is recommended that you speak to your health provider or contact a Women’s Health Physio for advice.
Can you contract your Pelvic Floor?
As we all navigate our way through the lockdown period, you may not have regular access to health services including Physiotherapy. This means you may not have the usual face to face checks that you otherwise would in clinic, to help assess if you are engaging your pelvic floor muscles.
Not all women will contract their muscles in the same way and research shows that many women do their pelvic floor exercises incorrectly and some find it hard to connect with these muscles at all. Furthermore, women with a Pelvic Organ Prolapse have been shown to have more difficulty in connecting with these muscles and activating them correctly.
A correct Pelvic Floor contraction must involve a squeeze and lift, normally starting from the back [or back passage], which works its way forward and up towards the bladder.
Firstly, start by sitting or lying down comfortably. It is important that you are relaxed and so placing cushions or pillows underneath your legs can help assist with this to begin with.
Now think about the opening of your back passage. Imagine that you feel the urge to pass wind, however you need to hold it. Initially squeeze the muscles around the opening of your back passage, whilst keeping your buttocks, inner thighs and tummy muscles relaxed [we only want to isolate those pelvic floor muscles].
Once you have got the initially squeeze, see if you can bring in the ‘lift’, whilst still keeping all of those other muscles relaxed. Feel the contraction lifting forwards and upwards towards your bladder, or to the opening where you pass urine, as though you were trying to stop the flow.
There are several common cues that can help you to contract your pelvic floor muscles correctly. Try a few of these different cues and see if there are any that work particularly well for you.
- Keep your pelvis still and imagine you are bringing your tailbone towards your pubic bone by drawing your pelvic floor muscles inwards and upwards. Make sure you don’t tilt your pelvis, you should not feel any movement occurring around your spine, hips or pelvic region.
- Visualise a jellyfish swimming, squeeze your pelvic floor by squeezing and lifting your back passage, as though the jellyfish is contracting, then relax as you imagine it to float through the water.
- Imagine you are picking up a blueberry with your back passage [squeeze], then gently draw it inside, lifting it forwards and upwards [lift].
- Imagine you are in an elevator. As you step in the door closes and you squeeze around your back passage, then visualise the elevator rising upwards and lift the pelvic floor upwards at the same time.
- Recent research has shown the most effective cue to help encourage a correct pelvic floor activation is to “Squeeze around your anus.”
As well as contracting the pelvic floor muscles, it is just as important to be able to relax them well. Make sure you relax fully in between each contraction, letting the muscle go as much possible before you contract again. We will discuss how to relax your pelvic floor for specific problems in more detail in a future blog post.

Things we don’t want when you are exercising your pelvic floor
- Increased tension anywhere else – bottom muscles, legs, tummy, shoulders, eyebrows etc. Try to keep the contraction relaxed!
- Make sure you are not bearing down. Some women push down into their pelvic floor instead of drawing upwards. You can use a mirror and take a look as you practise your contractions and if you see any bulging of your perineum or within your vagina, then stop.
- You should not experience pain during or after you practise your pelvic floor exercises. If you do, stop and contact a health professional [ideally a Women’s Health Physiotherapist].
- Make sure you are not holding your breath as you contract your pelvic floor muscles. This increases pressure within your tummy which can push down into the pelvic floor and make the exercise less effective and efficient. Try to exhale as you contract your pelvic floor muscles as this works with the body’s natural muscular action.
- Any worsening of symptoms eg pressure within your vagina, increased problems passing urine or stool, increased incontinence or any other unwanted symptoms, contact a Women’s Health Physiotherapist.
What if you just can’t feel anything or if you are unsure if you are doing the exercises correctly?
There are several tips you can use to check if you are activating your pelvic floor correctly. These include:
- Place a clean finger a few centimetres inside your vagina. As you contract your pelvic floor you should feel the muscles tighten around your finger and draw it gently up and in.
- You can use a mirror to check that you are not bearing down as you contract.
- You can try to squeeze around something such as a vibrator or your partner’s penis during intercourse.
- You can use biofeedback to help – The Pelvic Floor Educator [by Neen] is a cheap and effective way of determining if you are contracting your pelvic floor muscles.
Once you have connected with the muscles – what then?
Now you can hopefully contract your pelvic floor, you can build on this to form the basis of your own unique home exercise program, which has relevance to you and your individual ability. This program will need to be progressed and the muscles gradually loaded overtime.
- Activate your pelvic floor. How long can you hold the contraction for? This needs to be a relaxed hold, without you holding your breath or compensating [cheating] using other muscles. Make a note of how long you are able to hold the contraction for.
- How many repetitions can you achieve? Once you have held your contraction for as long as you can, let the muscles completely relax. Have a little rest [I initially recommend half of the total contraction hold time – for example if you held the contraction for 8 seconds, rest for 4 seconds]. Then repeat until you feel that the muscles start to become tired but are not completely fatigued. Make a note of how many you have managed to do in total.
- Perform fast contractions. These must be a full contraction to relaxation. I normally recommend aiming for a one second contraction with a one second rest. Make sure you don’t pulse the muscular contraction mid-range, instead make sure you relax fully and contract fully each time. Continue your fast contractions until the muscles feel as though they are starting to become tired but are not completely fatigued. Make a note of how many you have been able to do.
- Practise ‘automatic’ contractions of the pelvic floor. Each time you feel the urge to cough or sneeze, perform a ‘pre-activation’ of your pelvic floor just before you do so. This can also sometimes be enough to prevent any urinary leakage which may occur during these instances. This can take practise and repetition, particularly to become automatic and so be patient when practising this technique!
Progression…
Once you have mastered the above, it is important to try to progress yourself. You should find that over time you are able to hold each contraction for longer and that you can perform more repetitions. This is why noting down your reps and times every now and then is useful as you can visually see that you are progressing!
Positioning
I normally recommend to ladies to start practising pelvic floor exercises in lying with the knees bent up or in supported sitting. Once you can feel the squeeze and lift, you may wish to try the exercises in different functional positions such as sitting and standing. These positions progress the exercises by adding in gravitational forces and body weight, and so the muscles must work harder in order to activate. As a result, you may find that you are unable to do quite so many repetitions or hold for as many seconds to start with, once you progress into these positions.
Hold time
After a few weeks of practice, you should be able to hold each long, slow contraction for longer. Try to aim for 10 second holds initially, but if you feel you can hold for longer than this, add on a few more seconds!
Repetitions and Rests
With practice you should feel as though you can perform more repetitions over time. These must be good quality, with a full relaxation of the muscles in between. Makes sure you don’t cheat or use other muscles to compensate and if this is the case, it may be because the muscles are tiring and so this is a good point to stop. Try to aim for 10 long slow holds and 10 fast contractions initially but add on the reps as you progress.
You may also wish to reduce the rest time in between each of your long, slow contractions to reduce the recovery time in between.
Incorporate into functional exercise
Once you can perform your exercises well in standing, you can try adding in functional movements in standing to progress yourself further. Exercises such as squats, lunges and sitting to standing from a chair are examples of functional movements which we perform all day and so are useful to practice as a starting point.
You can try to gently engage your pelvic floor as you perform each exercise, along with an exhale to help encourage pressure management and normal pelvic floor activity. This is normally performed on the ‘effort’ during each exercise or when the body is working against gravity. Please note that if you experience any unwanted or worsening symptoms when practising these exercises, stop immediately.
Sit to Stand
Start off by sitting on the edge of a chair, with your feet on the ground and feet and knees hip width apart.
Take a breath in to prepare
As you exhale lean forward, gently activate your pelvic floor and push up into standing. You can cross your arms over your chest to bring the focus more into your legs.
Inhale, bend your knees and slowly lower yourself back down to sitting.
Repeat up to 10 repetitions.
Squat
Start in standing, with your feet and knees hip width part.
Inhale and bend your knees, lowering yourself into a squat position. Ensure your knees are angling over 2nd/3rd toe and are not sweeping inwards towards each-other. Keep your weight back onto your heels. You can reach your arms forwards or cross them over your chest.
Activate your pelvic floor gently and as you exhale push yourself back to a standing upright position.
Repeat up to 10 repetitions
Lunges
Standing with one foot in front of the other in a ‘step stance’. Ensure that both feet are pointing straight ahead and your pelvis is level. Lift the heel of the back foot away from the floor, bending the knee.
Keeping upright take a breath in and lower the back knee straight down towards the floor. The front knee will bend too but don’t bend this knee over the toes or lean forwards.
Activate your pelvic floor and exhale, returning to standing again.
Repeat up to 10 times on each leg.
Everyday activities
As well as performing each of these exercises individually, it is very useful to practise engaging your pelvic floor with activity throughout the day. Every-time you bend to pick something up, lift anything heavy, push, or pull, try to use your exhale with a pelvic floor activation as you perform the activity. The more you practise, the more automatic your pelvic floor activity will become, but remember this does take time!
Add Weight
Like any other muscle in the body, the pelvic floor responds to loading with weight. Weight can be applied with changes of position, using body weight or by adding weight training more specifically. You can hold some light weights whilst practising your exercises or when you practise the functional exercises below. Vaginal weights or cones can also be a useful way of applying resistance training to the pelvic floor and these will be discussed in a future blog post.

Conditions which may affect Pelvic Floor Function
There are several different factors which will influence your pelvic floor function on a daily basis, and these may help to explain why you feel more able to activate and exercise your pelvic floor at some times, compared with others.
- Time of day
Your pelvic floor muscles may tire as the day goes on and so exercising them towards the end of the day may be harder than the morning. I encourage women to exercise in the morning and try to complete all sets by lunchtime if possible! But if this doesn’t work for you, be mindful that exercising in the evening may not be as productive.
- Pelvic Health conditions
We know that pelvic health conditions such as incontinence, prolapse and constipation may influence how the pelvic floor works and your ability to activate it effectively. Bowel health and function is very important in pelvic health and will be discussed in a future blog post in more detail. As previously mentioned, not all women will activate the pelvic floor in the same way and so do check your technique is correct [more detail above] and if you have concerns seek further help.
- Pain
Some women have overactivity in their pelvic floor muscles. This is often linked with pelvic pain conditions, or chronic conditions including Endometriosis, Fibromyalgia or Bladder Pain Syndrome. Some conditions linked with anxiety or mental health may also result in tight and pelvic floor muscles. In these cases, pelvic floor exercises may be inappropriate or even, contraindicated forms of management and it is important that if you feel this may apply to you, to seek further guidance and to stop if you have any increase in your symptoms.
Summary
To summarise, not all women will activate their muscles the same and so adhering to generic advice in a leaflet may not be appropriate for all!
First, identify if you can activate and isolate your pelvic floor, then progress as you are able to do.
Take things gradually and try to be patient, strengthening does not occur overnight and your symptoms may take some time to improve, even with regular exercise.
Keep notes of how many reps and holds you can do – this will motivate you to continue with your exercises as you will see that you are improving!
Make sure you contact a Women’s Health Physiotherapist if you have problems. Face to face appointments are limited at the moment, but many practitioners are still offering virtual appointments and free advice via email or telephone. We are still here to support you!
And for anyone who wishes to do some ‘light’ reading 😊
References
- Henderson J.W, Wang S., Nygaard I. [2013]. Can women correctly contract their pelvic floor muscles without formal instruction? Female Pelvic Medicine and Reconstructive surgery 19[1] 8-12
- Joswick M, Joswick M [1998] The physiological basis of pelvic floor exercises in the treatment of stress urinary incontinence. British Journal of Obstetrics and Gynaecology. Vol. 105, pp. 1046-1051
- Bozkurt M, Yumru A.E, Sahin L. [2014] Pelvic floor dysfunction, and the effects of pregnancy and mode of delivery on the pelvic floor. Taiwanese Journal of Obstetrics and Gynecology. 53 452-458
- Pomian A, Lisik W, Kosierazdski M, Barcz E. [2016]. Obesity and Pelvic Floor Disorders: A review of the literature. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 1880-6
- Jain P, Parsons M, [2011] Review: The effects of obesity on the pelvic floor. The Obstetrician & Gynaecologist 13:133–142
- Subak L.L, Johnson C, Whitcomb E, Boban D, Saxton J, Brown JS [2002]. Does weight loss improve incontinence in moderately obese women? International Urogynecology Journal 13[1]40-43
- Lee J [2009]. The Menopause; Effects on the pelvic floor, symptoms and treatment options. Nursing Times; 105:48
- Folland J.P, Williams A.G [2007]. The adaptations to Strength Training. Morphological and Neurological contributions to increased strength. Sports Medicine 37[2]145-168
- National Institute for Health and Care Excellence [2019] Urinary Incontinence and Pelvic Organ Prolapse in Women: Management. NICE guideline [NG123].
- Dumoulin C, Cacciari LP, Hay-Smith EJC [2018]. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews. Issue 10. Art. No.: CD005654. DOI: 10.1002/14651858.CD005654.pub4.
- Bo K, Engh M, Majida M, Braekken I.H [2010]. Morphological changes after pelvic floor muscle training measured by 3-Dimensional Ultrasonography: A Randomized Controlled Trial. Obstetrics and Gynaecology. 115[2] 317-324